# Understanding Narcolepsy: Symptoms, Causes, and Treatment Options
Narcolepsy is a chronic sleep disorder characterized by overwhelming daytime drowsiness and sudden sleep attacks. It can affect anyone, but often begins in childhood or adolescence. Understanding narcolepsy is crucial for managing its symptoms and improving quality of life. Let’s dive into the symptoms, causes, and treatment options for this complex condition.
Narcolepsy is a neurological disorder that affects your ability to wake and sleep. People with narcolepsy may experience excessive daytime sleepiness and uncontrollable episodes of falling asleep, known as sleep attacks, at inappropriate times such as during work or school.
Symptoms of Narcolepsy
Understanding the symptoms of narcolepsy is the first step in managing the condition effectively. The four major symptoms are excessive daytime sleepiness, cataplexy, sleep paralysis, and hallucinations.
Excessive Daytime Sleepiness
Excessive daytime sleepiness is the most common symptom of narcolepsy. It refers to an overwhelming feeling of tiredness and a persistent desire to sleep throughout the day, regardless of how much rest you get at night.
Cataplexy
Cataplexy is a sudden, brief loss of muscle tone or strength that can be triggered by intense emotions such as laughter, surprise, or anger. This can result in slurred speech, buckling knees, or even complete collapse.
Sleep Paralysis
Sleep paralysis occurs when you temporarily cannot move or speak while falling asleep or waking up. These episodes can last from a few seconds to a couple of minutes and are often frightening.
Hallucinations
Hallucinations in narcolepsy are vivid and often frightening. They can occur while falling asleep (hypnagogic) or waking up (hypnopompic) and are sometimes difficult to distinguish from reality.
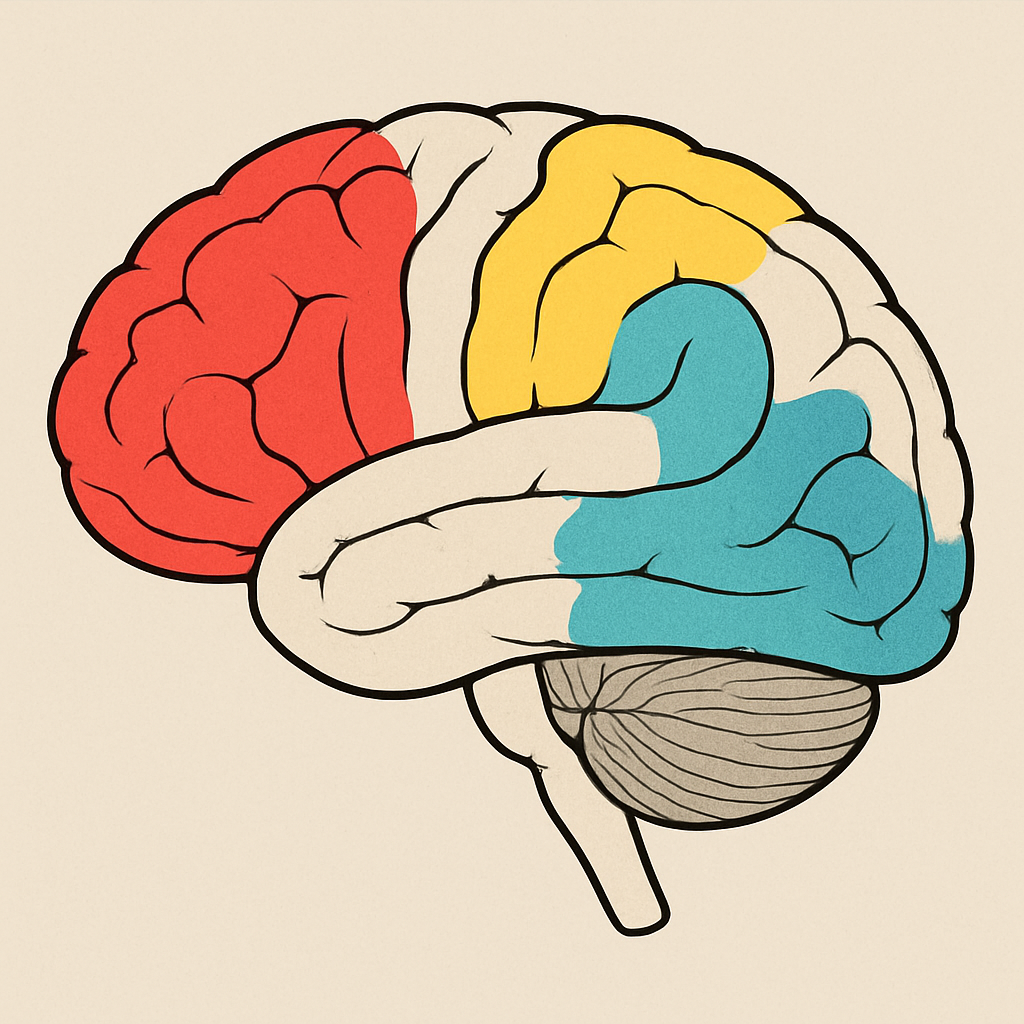
Causes of Narcolepsy
The exact cause of narcolepsy is unknown, but researchers believe it may be linked to several factors. The most significant of these is the loss of a brain chemical called hypocretin, which regulates wakefulness and REM sleep.
Genetic Factors
Genetics play a role in narcolepsy. While it is not directly inherited, certain genetic factors can increase susceptibility to the disorder.
Autoimmune Response
Some researchers believe narcolepsy may be triggered by an autoimmune response, where the body’s immune system mistakenly attacks healthy cells, including those that produce hypocretin.
Brain Injuries and Infections
In rare cases, narcolepsy can be triggered by a brain injury or neurological condition affecting areas of the brain that regulate sleep and wakefulness.
Diagnosis of Narcolepsy
Diagnosing narcolepsy involves a thorough evaluation by a sleep specialist. The process typically includes a detailed medical history, physical exam, and sleep study tests.
Sleep Study Tests
Two main tests are used to diagnose narcolepsy:
- Polysomnogram (PSG): Conducted overnight, this test records brain activity, muscle movements, breathing, and eye movements during sleep.
- Multiple Sleep Latency Test (MSLT): Conducted the day after a PSG, this test measures how quickly you fall asleep in a quiet environment during the day.
Additional Evaluations
In some cases, additional tests such as blood tests or imaging studies may be conducted to rule out other conditions that could be causing the symptoms.
Narcolepsy Treatment Options
While there is no cure for narcolepsy, several treatments can help manage symptoms and improve quality of life. Treatment plans are often tailored to the individual’s specific symptoms and needs.
Medications
Narcolepsy medications can help control symptoms. Stimulants are commonly prescribed to combat excessive daytime sleepiness, while antidepressants can help manage cataplexy and other symptoms.
- Stimulants: Drugs like modafinil or armodafinil can promote wakefulness.
- Antidepressants: Certain antidepressants can help control cataplexy, sleep paralysis, and hallucinations.
- Sodium Oxybate: This medication can help improve nighttime sleep and control cataplexy.
Lifestyle Modifications
Lifestyle changes can significantly impact narcolepsy management. Establishing a regular sleep schedule, taking short naps, and practicing good sleep hygiene can help manage symptoms.
Behavioral Therapy
Cognitive behavioral therapy (CBT) can provide strategies to cope with the emotional and psychological aspects of living with narcolepsy.
by Who’s Denilo ? (https://unsplash.com/@whoisdenilo)
Narcolepsy Management and Support
Managing narcolepsy involves a combination of medical treatment and lifestyle adjustments. Support from healthcare professionals, family, and friends can make a significant difference.
Staying Informed
Educating yourself and your loved ones about narcolepsy can empower you to manage the condition more effectively. Joining support groups and connecting with others who have narcolepsy can also provide valuable insights and encouragement.
Work and School Accommodations
People with narcolepsy may need accommodations in the workplace or at school. This can include flexible schedules, designated nap times, or a quiet space for rest.
Conclusion
Narcolepsy is a lifelong condition that requires careful management. By understanding its symptoms, causes, and treatment options, those affected by narcolepsy can lead fulfilling lives. If you suspect you or someone you know may have narcolepsy, consult a healthcare professional for a comprehensive evaluation and personalized treatment plan.